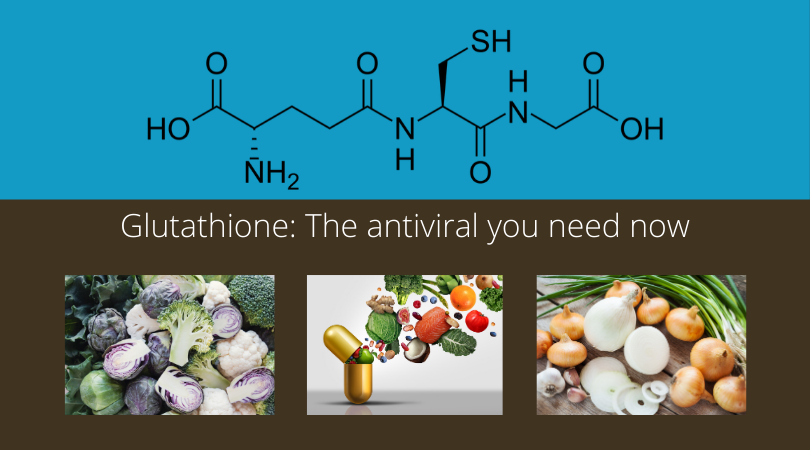
Glutathione: The antiviral you need now
UPDATE: Newly published!
Endogenous Deficiency of Glutathione as the Most Likely Cause of Serious Manifestations and Death in COVID-19 Patients
“Glutathione deficiency is an acquired condition attributable to decreased biosynthesis and/or increased depletion of the endogenous GSH pool influenced by risk factors such as aging, male sex, comorbidity, and smoking alone or in combinations. Glutathione deficiency in COVID-19 patients with serious illness may also be a result of decreased consumption of fresh vegetables and fruits (especially during winter and spring seasons), which contributes to over 50% of dietary glutathione intake. The hypothesis suggests that SARS-CoV-2 virus poses a danger only for people with endogenous glutathione deficiency, regardless which of the factors aging, chronic disease comorbidity, smoking or some others were responsible for this deficit. The hypothesis provides novel insights into the etiology and mechanisms responsible for serious manifestations of COVID-19 infection and justifies promising opportunities for effective treatment and prevention of the illness through glutathione recovering with N-acetylcysteine and reduced glutathione.
Since the antiviral effect of glutathione is nonspecific, there is reason to believe that glutathione is also active against SARS-CoV-2. Therefore, restoration of glutathione levels in COVID-19 patients would be a promising approach for the management of the novel coronavirus SARS-CoV-2. Notably, long-term oral administration of N-acetylcysteine has already been tested as an effective preventive measure against respiratory viral infections.1 N-Acetylcysteine is widely available, safe, and cheap and could be used in an “off-label” manner. Moreover, parenteral injection of NAC or reduced glutathione (GSH is more bioavailable than NAC) could be an efficient therapy for COVID-19 patients with serious illness. Horowitz et al.18 just published a paper confirming this hypothesis: the authors reported the efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia.”
A new case study shows promise for glutathione to treat COVID-19 symptoms
Efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia: A report of 2 cases
“NAC, alpha-lipoic acid and GSH all inhibit TNF-α-induced NF-kappaB activation. Oral and IV glutathione as well as glutathione precursors (N-acetyl-cysteine, alpha-lipoic acid) may, therefore, represent a novel treatment approach for blocking NFKappaB and addressing “cytokine storm syndrome” and respiratory distress in patients suffering with COVID 19 pneumonia. Zinc, vitamin C and NRF 2 activators may also be helpful in decreasing the inflammatory response and lowering cytokine production.”
Glutathione (GSH) is a peptide (smaller versions of proteins) that contains one amino acid residue each of glutamic acid, cysteine, and glycine. These are found in plants and animal tissue, but we often don’t get enough of them because they are easily destroyed by cooking. Additionally, glutathione is used rapidly by exposure to toxins, infections, and some pharmaceuticals, leaving us depleted when we need it the most. Supplementation is essential during these critical times of depletion.
“Reduced secretion of Th1 cytokines, which is associated with GSH depletion, could weaken the host defenses against viral infections.” (PMID: 32123833)
Glutathione “is essential for the viability and function of virtually all cells” (PMID: 9050888).
Glutathione reduces viral replication. (PMID: 32123833).
Dr. Edward Fogarty says, “Precursors to GSH are antiviral software for every cell.”
-
Precursors are the building blocks your body needs to synthesize glutathione: glutamic acid, cysteine, and glycine.
-
Precursor supplements: Pro Immune 200, a patented product by Dr. Crum, contains all 3 key amino acids needed;
-
N-acetylcysteine (NAC) is the amino acid most critical to replace and is available from many companies as a supplement. Hospitals stock it to treat acetaminophen overdose.
-
For precursor foods, nutrients, and lifestyle choices that boost glutathione, please see this excellent article by Dr. Hyman: Essential Glutathione: The Mother of All Antioxidants
Warning: Acetaminophen (Tylenol, paracetamol, and found in many cold and flu remedies) depletes glutathione.
Some science to explore:
Georgia State Researchers Discover Novel Antiviral Shuts Down Replication Of Zika Virus Inside Human Cells – Georgia State University News
“A unique formulation of multiple amino acids inhibits the replication of Zika virus by up to 90 percent in human and non-human primate cells, according to a study led by Georgia State University.
The study authors tested a novel formulation of three free-form amino acids (FFAAP)—cystine, glycine and glutamate, as well as a minute amount of selenium—that was previously known to increase biosynthesis (or production) of glutathione, an antioxidant, within cells. Intracellular glutathione has been shown to adversely affect certain viruses, including HIV, suggesting that it could be an active cell defense.”
PMID: 30217651 A Novel Antiviral Inhibits Zika Virus Infection While Increasing Intracellular Glutathione Biosynthesis in Distinct Cell Culture Models
Abstract
We investigated the effects of a specific free-form amino acids formulation on Zika virus replication in two different cell culture model systems, one representative of humans and the other of Old World primates from whom Zika virus was first isolated. Here we present data demonstrating that the formulation of the specific free-form amino acid (FFAAP), comprising cystine, glycine, and a glutamate source, along with a minute concentration of selenium inhibited Zika virus replication by up to 90% with an ED90 (effective dose at which 90% of a dose of Zika virus was inhibited) of 2.5 mM in human cells and 4 mM Vero cells. The ED90 concentration of precursors was innocuous for uninfected cells, but resulted in reduced Zika virus replication by up to 90% at 2-5 mM concentrations in nonhuman primate cells and at 1-3 mM concentration in human placental cells. Two important observations were forthcoming: 1) Zika virus production was decreased by up to 90% in Vero and JEG-3 cells treated with FFAAP (ED90 4.0 mM, and 2.5 mM, respectively) throughout 48-72 h of post infection (hpi) compared to untreated infected cells and 2) Zika virus requires intracellular glutathione for replication in human placental cells, while showing enhanced replication in Vero cells with no glutathione. Relative increases in intracellular glutathione biosynthesis followed FFAAP treatment but blocking intracellular biosynthesis of glutathione in human cells resulted in virus inhibition in human placental cells. The blockade of biosynthesis actually increased Zika virus replication in Vero cells. These findings identify an efficacious inhibitor, FFAAP, of Zika virus replication in both human and nonhuman primate cells, while providing novel insight into the different roles of intracellular glutathione in Zika virus replication.
PMID: 9050888 Glutathione deficiency is associated with impaired survival in HIV disease
Abstract
Glutathione (GSH), a cysteine-containing tripeptide, is essential for the viability and function of virtually all cells. In vitro studies showing that low GSH levels both promote HIV expression and impair T cell function suggested a link between GSH depletion and HIV disease progression. Clinical studies presented here directly demonstrate that low GSH levels predict poor survival in otherwise indistinguishable HIV-infected subjects. Specifically, we show that GSH deficiency in CD4 T cells from such subjects is associated with markedly decreased survival 2–3 years after baseline data collection (Kaplan–Meier and logistic regression analyses, P < 0.0001 for both analyses). This finding, supported by evidence demonstrating that oral administration of the GSH prodrug N-acetylcysteine replenishes GSH in these subjects and suggesting that N-acetylcysteine administration can improve their survival, establishes GSH deficiency as a key determinant of survival in HIV disease. Further, it argues strongly that the unnecessary or excessive use of acetaminophen, alcohol, or other drugs known to deplete GSH should be avoided by HIV-infected individuals.
PMID: 32123833 Glutathione increase by the n‐butanoyl glutathione derivative (GSH‐C4) inhibits viral replication and induces a predominant Th1 immune profile in old mice infected with influenza virus
Abstract
During aging, glutathione (GSH) content declines and the immune system undergoes a deficiency in the induction of Th1 response. Reduced secretion of Th1 cytokines, which is associated with GSH depletion, could weaken the host defenses against viral infections. We first evaluated the concentration of GSH and cysteine in organs of old mice; then, the effect of the administration of the N‐butanoyl GSH derivative (GSH‐C4) on the response of aged mice infected with influenza A PR8/H1N1 virus was studied through the determination of GSH concentration in organs, lung viral titer, IgA and IgG1/IgG2a production, and Th1/Th2 cytokine profile. Old mice had lower GSH than young mice in organs. Also the gene expression of endoplasmic reticulum (ER) stress markers involved in GSH metabolism and folding of proteins, that is, Nrf2 and PDI, was reduced. Following infection, GSH content remained low and neither infection nor GSH‐C4 treatment affected Nrf2 expression. In contrast, PDI expression was upregulated during infection and appeared counterbalanced by GSH‐C4. Moreover, the treatment with GSH‐C4 increased GSH content in organs, reduced viral replication and induced a predominant Th1 response. In conclusion, GSH‐C4 treatment could be used in the elderly to contrast influenza virus infection by inducing immune response, in particular the Th1 profile.
PMID: 27147856 A Review of the Evidence Concerning Hepatic Glutathione Depletion and Susceptibility to Hepatotoxicity After Paracetamol Overdose
Abstract
Paracetamol (acetaminophen) poisoning is common throughout the world. The management of nonstaggered (acute) paracetamol overdose is based on the plasma paracetamol concentration plotted on a treatment nomogram. In the UK there are two treatment lines on this nomogram, with the lower treatment line used for individuals felt to be at ‘high risk’ of paracetamol-related hepatotoxicity either as a result of induction of cytochrome P450 isoenzymes or reduction of intrahepatic glutathione. In this article we review the risk factors that, in current guidelines, are felt to increase risk due to a reduction in intrahepatic glutathione concentrations. Based on our review of the published literature, we feel that cystic fibrosis, acute viral illness, malnutrition, and eating disorders such as anorexia nervosa are likely to be associated with reduction in intrahepatic glutathione concentrations, and that this risk is likely to be related to malnutrition secondary to the disease. Chronic hepatitis C infection is also associated with reduced glutathione concentrations, although this appears to be independent of any associated malnutrition. Ageing and acute fasting are not associated with an increased risk of paracetamol-related hepatotoxicity due to reductions in glutathione concentrations. Finally, the evidence for HIV infection is inconclusive, particularly as the majority of studies were conducted in the pre-anti-viral treatment (HAART) era; however it is likely that patients with symptomatic HIV/AIDS have reduced glutathione concentrations due to associated malnutrition. Although there have been few studies which have specifically investigated whether there is an association between reduced intrahepatic glutathione concentrations and increased risk of paracetamol-related hepatotoxicity, in our opinion, it is likely that the above conditions that are associated with reduced glutathione concentrations, will be associated with an increased risk of paracetamol-related hepatotoxicity.
PMID: 19953420 Bacterial- And Viral-Induced Inflammation Increases Sensitivity to Acetaminophen Hepatotoxicity
Abstract
Acetaminophen (APAP)-induced hepatotoxicity accounts for nearly half of acute liver failure cases in the United States. The doses that produce hepatotoxicity vary considerably and many risk factors have been proposed, including liver inflammation from viral hepatitis. Interestingly, inflammatory stress from another stimulus, bacterial endotoxin (lipopolysaccharide, LPS), renders the liver more sensitive to hepatotoxicity from numerous xenobiotic agents. The purpose of these studies was to test the hypothesis that inflammation induced by LPS or infection with reovirus increases sensitivity to APAP-induced liver injury. For LPS-induced inflammation, C57BL/6J mice were treated with either saline or LPS (44 x 10(6) EU/kg, ip) 2 h before treatment with APAP (100-400 mg/kg, ip) or saline. No elevation in serum alanine aminotransferase (ALT) activity was observed in mice that received vehicle or LPS alone. LPS co-treatment produced a leftward shift of the dose-response curve for APAP-induced hepatotoxicity and led to significantly greater tumor necrosis factor-alpha (TNF) production than APAP alone. Reovirus serotype 1 (10(8) PFU, iv) induced inflammation in Balb/c mice as evidenced by increases in hepatic mRNAs for macrophage inhibitory protein-2, interleukin-6, and TNF. Co-administration of reovirus and APAP at doses of 450 and 700 mg/kg (2 h after reovirus) led to increases in serum ALT activity, whereas neither reovirus nor APAP alone produced liver injury. Consistent with the increases in serum ALT activity, histopathologic examination revealed centrilobular necrosis with marked neutrophilic accumulation only in livers of mice treated with LPS/APAP or with reovirus/APAP. The results suggest that normally noninjurious doses of APAP are rendered hepatotoxic by modest inflammation, whether bacterial or viral in origin.
PMID: 31116598 Antipyretic drugs in patients with fever and infection: literature review
Abstract
Background: antipyretic drugs are routinely administered to febrile patients with infection in secondary care. However, the use of antipyretics to suppress fever during infection remains a controversial topic within the literature. It is argued that fever suppression may interfere with the body’s natural defence mechanisms, and may worsen patient outcomes.
Method: a literature review was undertaken to determine whether the administration of antipyretic drugs to adult patients with infection and fever, in secondary care, improves or worsens patient outcomes.
Results: contrasting results were reported; two studies demonstrated improved patient outcomes following antipyretic administration, while several studies demonstrated increased mortality risk associated with antipyretics and/or demonstrated fever’s benefits during infection. Results also demonstrated that health professionals continue to view fever as deleterious.
Conclusion: the evidence does not currently support routine antipyretic administration. Considering patients’ comorbidities and symptoms of their underlying illness will promote safe, evidence-based and appropriate administration of antipyretics.
PMID: 11130213 Effect of Antipyretic Therapy on the Duration of Illness in Experimental Influenza A, Shigella sonnei, and Rickettsia ricketts infections
Abstract
Study Objectives. To determine whether antipyretic therapy prolongs the course of experimental influenza A, Shigella sonnei, and Rickettsia rickettsii infections.
Design. Retrospective observational study.
Setting. University Center for Vaccine Development.
Subjects. Fifty‐four volunteers with experimentally induced influenza A, 45 with S. sonnei, and 21 with R. rickettsii infections participated.
Interventions. Subjects from the six influenza A studies were challenged intranasally. If they met certain criteria, they were offered aspirin or acetaminophen for symptomatic relief. Subjects from the three Shigella studies were challenged with the bacteria and then given trimethoprim‐sulfamethoxazole. Acetaminophen also could be administered. In the one R. rickettsii trial, subjects were inoculated intradermally and treated with tetracycline. Again, acetaminophen was administered for symptomatic relief.
Measurements and Main Results. Data, excerpted from subjects’ study records, were evaluated using Wilcoxon tests, Spearman’s correlation coefficients, and multiple regression analysis. Two‐tailed hypotheses with a value of 0.05 were used for all of the analyses. There was a striking correlation between antipyretic therapy and duration of illness in subjects infected with influenza A and S. sonnei, but not R. rickettsii.
Conclusions. Multivariate analysis suggested that antipyretic therapy prolonged illness in subjects infected with influenza A, but its use was the result of prolonged illness in those infected with S. sonnei. The precise nature of these relationships requires a prospective, randomized, placebo‐controlled trial.
PMID:2172402 Adverse effects of aspirin, acetaminophen, and ibuprofen on immune function, viral shedding, and clinical status in rhinovirus-infected volunteers.
Abstract
A double-blind, placebo-controlled trial was conducted to study the effects of over-the-counter analgesic/antipyretic medications on virus shedding, immune response, and clinical status in the common cold. Sixty healthy volunteers were challenged intranasally with rhinovirus type 2 and randomized to one of four treatment arms: aspirin, acetaminophen, ibuprofen, or placebo. Fifty-six volunteers were successfully infected and shed virus on at least 4 days after challenge. Virus shedding, antibody levels, clinical symptoms and signs, and blood leukocyte levels were carefully monitored. Use of aspirin and acetaminophen was associated with suppression of serum neutralizing antibody response (P less than .05 vs. placebo) and increased nasal symptoms and signs (P less than .05 vs. placebo). A concomitant rise in circulating monocytes suggested that the suppression of antibody response may be mediated through drug effects on monocytes and/or mononuclear phagocytes. There were no significant differences in viral shedding among the four groups, but a trend toward longer duration of virus shedding was observed in the aspirin and acetaminophen groups.
PMID: 2656959 Acetaminophen: More harm than good for chickenpox?
Study objective To determine whether acetaminophen affects the duration or severity of childhood varicella.
Design: Randomized, double-blind, placebo-controlled trial.
Setting: Office- and hospital-based pediatric practices.
Patients: Seventy-two children between 1 and 12 years of age entered the study. One child was withdrawn because of high fever, and three children did not complete the study; 31 received placebo and 37 received acetaminophen.
Interventions: Acetaminophen, 10 mg/kg/dose, was given at 8 am, 12 pm, 4 pm, and 8 pm for 4 days. Placebo was given to the control group. Itching, appetite, activity, and overall condition were measured for 6 days. The time to last vesicle formation, time to total scabbing, and time to total healing were measured until complete resolution of the exanthem.
Measurements and main results: The following results were better in the placebo group (p<.05): time to total scrabbing 5.6 days (SD 2.5) versus 6.7 days (SD 2.3) in the acetaminophen group, and itching on day 4 in the placebo group (symptom score 2.9 (SD 0.20) vs 2.2 (SD 0.26)). Activity was better in the acetaminophen group on day 2 (3.13 (SD 0.23) vs 2.82 (SD 0.24))
Conclusions: These results provide evidence that acetaminophen does not alleviate symptoms in children with varicella and may prolong illness.
- PMID: 8540746 Evidence for antiviral activity of glutathione: in vitro inhibition of herpes simplex virus type 1 replication.
Abstract
The role of glutathione (GSH) in the in vitro infection and replication of human herpes simplex virus type 1 (HSV-1) was investigated. Intracellular endogenous GSH levels dramatically decreased in the first 24 h after virus adsorption, starting immediately after virus challenge. The addition of exogenous GSH was not only able to restore its intracellular levels almost up to those found in uninfected cells, but also to inhibit > 99% the replication of HSV-1. This inhibition was concentration-dependent, not related to toxic effects on host cells and also maintained if the exogenous GSH was added as late as 24 h after virus challenge, i.e. when virus infection was fully established. Electron microscopic examination of HSV-1-infected cells showed that GSH dramatically reduced the number of extracellular and intracytoplasmic virus particles, whereas some complete nucleocapsids were still detected within the nuclei of GSH-treated cells. Consistent with this observation, immunoblot analysis showed that the expression of HSV-1-glycoprotein B, crucial for the release and the infectivity of virus particles, was significantly decreased. Data suggest that exogenous GSH inhibits the replication of HSV-1 by interfering with very late stages of the virus life cycle, without affecting cellular metabolism.